From sleeping on staircases and bare floors to battling mosquitoes, rain, and exhaustion, relatives of patients admitted to teaching hospitals across the country are enduring harsh realities as they care for their loved ones. With no accommodation provided for them, many spend sleepless nights in unsafe and unhealthy conditions. JANET OGUNDEPO reports
A little after 2 am one night in October, a Sokoto-based businessman and new father, A. O. Yusuf, rushed his wife to the Usmanu Danfodiyo University Teaching Hospital, Sokoto.
His wife had developed complications after giving birth some weeks earlier. Taking her to the hospital and getting her stabilised was his priority; he could not plan for anything beyond ensuring she received treatment.
Thankful for the immediate care his wife received, Yusuf said he was relieved she was finally out of danger, but fatigue pushed him to sit and doze off on an empty bed.
After some minutes, a nurse woke him up and told him to leave the ward.
Outside, heavy rain pounded the hospital grounds, and Yusuf said he pleaded for just two hours to rest his head, assuring the nurse he would get up before doctors resumed their ward rounds.
“Get out, I don’t care,” was the response that greeted him.
With nowhere to go and no provision for patient relatives to shelter, Yusuf stepped into the cold night. He had no wrapper, mat, or dry corner to sit on.
“That night was traumatic for me. There was no lodge, no place to hide from the rain. I did not have anything to lie on the ground. I just kept walking around the compound until morning,” he added.
Desperate for temporary refuge, he said he approached a police patrol van parked nearby and begged to sit inside until dawn. The officers refused. From then till daybreak, Yusuf walked the length of the hospital grounds in soaked clothes, shivering and exhausted.
By morning, he had not slept for a minute.
Other relatives he met during his stay slept on staircases, wooden benches, or bare concrete. Many battled mosquitoes, cold, and filthy surroundings.
The few toilets around were either locked or too dirty, the new father said.
“The sanitation is terrible. Most of the time, even patients complain that the toilets are not clean. For relatives, it is even worse. I used the bush to urinate because the toilets were not usable,” he recounted.
After spending five days at the hospital, Yusuf said he fell ill the moment he got home.
“I treated myself for one week. I could not go to work for three days and then managed to resume half a day for about a week,” he said.
His absence from work cost him days of lost income and weeks of reduced productivity.
For him and for many Nigerians caring for sick relatives, the lack of designated resting places in hospitals is more than an inconvenience; it is a growing public health risk.
“There is zero arrangement for patient relatives. If they do not want us inside the ward, they should create a place where we can rest. Even if we have to pay, let there be a clean room, a small mattress, and a mosquito net. Some of us are willing to pay. People cannot keep sleeping on the ground,” the businessman noted.
Further recounting his five-day hospital stay, Yusuf said while he was sleep-deprived and fatigued, he was stretched to breaking point over payment processes.
“In 2025, you imagine people still going to queue just to make payments. You trek 100 metres, 200, even up to 500 metres or one kilometre inside the hospital to get things done, and by the time you finish, you are already exhausted before your patient even starts receiving treatment,” he said.
Yusuf commended the doctors for their kindness and responsiveness, but said the system itself was draining.
Yusuf’s experience happened less than a month ago. It is only one of many.
We slept like animals’
For Tochukwu, who spent nearly two months caring for a stroke patient at the University College Hospital, Ibadan, the nights were not just uncomfortable; they were dehumanising.
He spent the first month staying through the night beside the patient, and the second month alternating with his brother, but the fatigue never let up.
His daily responsibilities were endless.
Feeding, cleaning, bathing, getting drugs, and taking samples to different departments where they would be tested. It was a stroke patient, so everything depended on us,” he recounted.
With no accommodation for caregivers, nights were a battle for survival.
“There was no room for caregivers to sleep. Everyone scrambled for space in the corridors leading to the entrance of the ward. You either sleep on the floor or sleep sitting,” he said.
For Tochukwu, the staircase became his makeshift bed.
“Most nights, I slept sitting on the staircase leading to the floors of the different wards. The cold, the mosquitoes… We slept like animals out in the cold. It was a terrible time and an awful experience,” he said.
Continuing, he said, “Health-wise, I broke down after the whole episode. I was sick for a while and the traces of the mosquito bites can still be seen around my arms and legs.
“You know I can’t just break down because I had someone to care for, so I pushed my body extra. I had malaria and also fatigue because of all the stress.
“The toilets were clean only on mornings when the cleaners came and by evening, there were always pools of water on the floor from leaking pipes.”
Aside from the lack of a relatives’ lodge, the rigid payment processes were another burden.
Because Tochukwu’s relative was not on the National Health Insurance Scheme, the financial strain deepened his stress.
The diehard Liverpool fan urged the hospital management to “provide well-fumigated rooms where caregivers can sleep. Mosquito nets can be used when fumigation is expensive. Also, all corridors and balconies of hospital wards should be covered with mosquito nets.”
Why relatives’ lodges are necessary
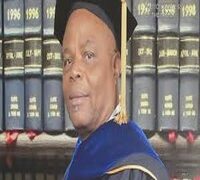
A Professor of Public Health at the University of Ilorin, Ilorin, Kwara State, Tanimola Akande, said caregivers or relatives have a lot of roles to play in the care of admitted patients, especially in public hospitals.
He explained that their presence was necessary because they perform tasks that require constant movement around the hospital on behalf of their patients.
The don noted that the need for patient relatives in hospitals has grown largely “due to the failure of public health facilities’ service. There is a massive shortage of hospital staff who are supposed to perform these roles, particularly in public hospitals. This is hardly the case in big private hospitals.”
Akande asserted, “It is therefore necessary for the relatives to be around the hospital and the need for patients’ relations to lodge in these hospitals.”
Also, a public health reform advocate, Ayo Adebusoye, said that family caregivers are an integral, if unofficial, part of care in Nigerian public hospitals, responsible for feeding patients, sourcing consumables and advocating for timely treatment.
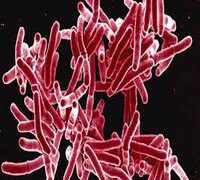
He noted that when caregivers sleep on corridor floors or in cars, it worsens patient safety because “sleep-deprived, exhausted caregivers miss instructions and make errors with feeding/medications. Sleep loss also impairs immunity, increasing infection risk for the caregiver and, by extension, the patient.”
He added, “Overcrowded waiting areas and makeshift sleeping spaces without hand-hygiene facilities or clean toilets undermine infection prevention and control. WHO/UNICEF data show low WASH coverage in health facilities across sub-Saharan Africa, with only about 60 per cent having basic water services and just about 34 per cent having basic hygiene; waste management and sanitation are even weaker in many contexts. That reality maps directly to dirty toilets and absent handwashing points for caregivers.”
Adebusoye noted that the absence of such facilities also creates an equity problem, as many families cannot afford nearby hotels.
“Providing a modest, clean, affordable place to sleep, wash, pray, store belongings, and receive Infection Prevention and Control orientation is not a luxury; it’s core to patient outcomes and humane care,” he asserts.
In a study on informal caregivers in Nigerian hospitals by Kudus Adebayo et al, family relatives and friends of hospitalised patients, known as informal caregivers, have become an essential but invisible workforce, filling huge gaps created by staff shortages and service inefficiencies.
The study reveals that these caregivers face severe health and well-being challenges, often worsened by the conditions under which they are forced to stay.
“Many sleep in corridors, open spaces and other makeshift spots because hospitals provide no accommodation. As a result, they report stress, weakness, pain, sleeplessness, poor feeding, mental strain, and a heightened risk of infections. The environment itself exposes them to harsh weather, foul odours, and unsafe toilets, with limited access to water or hygiene facilities,” it revealed.
It also showed that caregivers suffer social and financial strain, from loss of income and religious routines to indebtedness and the high cost of lengthy hospital stays. Security concerns, harassment, theft, and unsafe nighttime sleeping conditions compound their vulnerability.
The study stresses that these experiences are not merely inconveniences but reveal systemic gaps in Nigeria’s health service delivery.
It concluded that hospital managers and policymakers must recognise caregivers as key actors in patient care and urgently create interventions, such as safe resting areas, improved hygiene facilities and caregiver support structures, to protect their physical and mental well-being.
Who is responsible for providing the lodges
Hospital Management and Boards and Teaching Hospital authorities hold the operational mandate to ensure safe, humane environments and to integrate caregiver accommodation into capital plans and Public Private Partnership pipelines,” the Chairman of the Board of Trustees of the Public Health Sustainable Advocacy Initiative, Adebusoye, said.
He noted that the National Health Act 2014 sets standards for service delivery and empowers authorities to organise services.
The public health advocate added that the IPC expectations from the Nigeria Centre for Disease Control and Prevention further require facilities to enable safe visitor practices, which is impossible without decent WASH and managed spaces.
He urged state Ministries of Health and regulators to enforce minimum facility standards and align with the Patients’ Bill of Rights ethos of dignity, cleanliness and information.
Adebusoye called for the involvement of the private sector and Corporate Social Responsibility initiatives, as well as philanthropy, Rotary and faith-based groups, noting that they have proven to be reliable partners in financing and donating caregiver lodges and essential equipment.
He said such partnerships, which have already delivered models like the relatives’ lodge at the Lagos State University Teaching Hospital, Ikeja, could help replicate similar facilities across tertiary and high-volume hospitals.
At UCH
Findings by PUNCH Healthwise showed that the Catholic Mission, in November 2024, commissioned a waiting lounge known as the Caritas Waiting Lounge for relatives of patients in the emergency ward at the University College Hospital, Ibadan, Oyo State.
A staff member who spoke to PUNCH Healthwise said the centre was originally designed as a daytime waiting area for caregivers.
However, a month after it opened, relatives needed the space more at night.
“The centre was then tested for two weeks as a night-time shelter before it was officially opened for overnight use. Caregivers now rent big hard cartons for N500 and mats for N1,000, which are laid out between the benches,” she noted.
The facility has constant electricity and inverters to support uninterrupted power.
PUNCH Healthwise also learnt that UCH runs another small accommodation called Alaanu House, designated for relatives whose patients are on admission in the wards.
However, the rooms are few, leaving many caregivers sleeping in corridors and staircases.
The facility is managed by the hospital and linked to the Medical Social Work department, which verifies referrals to ensure only relatives of admitted patients access the space. The nightly rate varies by hospital discretion, but discharged patients’ relatives reported paying between N200 and N400.
Mosquitoes, stress, and trauma
Another caregiver at the University College Hospital, Ibadan, who asked not to be named, said their family spent three weeks caring for a critically ill relative and endured “an experience I don’t wish for anyone.”
The relative said the family was responsible for “everything the woman needed,” including food, drugs, saline, syringes, gloves and other consumables. But the absence of a proper resting place pushed them to the breaking point.
“There was nothing put in place for people taking care of patients,” the caregiver said. “There was nowhere to sleep or even rest during the day.”
She described the corridor chairs as so small and inadequate that many caregivers stood for hours because all available seats were taken.
The toilet situation, she added, made the stay even more distressing. “Sometimes we had to buy water because there was no light to pump water,” she said. On some days, caregivers were barred from using the toilets entirely.
She said the hospital’s policy on caregivers staying overnight forced them into unsafe conditions.
“They don’t allow you to stay with your patient, yet they’ll ask you to go outside to the corridor and sleep, and the mosquitoes there are terrible,” she said.
Eventually, constant exposure to cold, mosquitoes, and physical exhaustion forced the family to return home each night and resume care at dawn. But the emotional cost lingered.
“It affected all of us terribly. I had trauma for months. Whenever we remember the experience, we just pray and say, ‘God, never again,’” she said.
Slept for three days after discharge
After spending three days at one teaching hospital in Lagos, a middle-aged man, Ayotunde Quadri (not real name), said he slept for three days after discharge.
Falling sick is an understatement. After my relative was discharged, all I did was eat, sleep and wake up for three days. The distance from one spot to the other took a toll on me and my sister.
“There was a normal waiting lounge with long benches, but not really suitable for sleeping on. But while waiting for three days, we managed to sleep on it,” Quadri told PUNCH Healthwise.
Findings reveal that many public hospitals around the country lack designated and properly built patient relatives’ lodges and waiting areas, leaving many caregivers sleeping in cars, roaming the hospital, or sitting and standing by walkways and corridors.
Apart from the stressful conditions, experts say such caregivers are exposed to infections.
Prioritise your health
Reacting to complaints from caregivers who fall ill due to poor sleeping spaces, exposure to infection and unhygienic conveniences, Akande said the environment they operate in makes them vulnerable.
“The burden of care, the running around and the environment they are exposed to make them susceptible to illnesses. It is therefore necessary to provide an appropriate patient relations lodge that can be paid for. Most importantly, hospitals should be adequately staffed and provide quality health care services to reduce the need for relatives to always hang around to care for their loved ones,” the public health expert said.
Akande advised caregivers to prioritise their own health while supporting their loved ones.
“Relatives should be mindful of the hospital environment and take precautions such as using appropriate clothing, sharing responsibilities to reduce physical burden, and taking the opportunity to also receive medical care when necessary,” he explained.
While many public hospitals have visiting-hour policies, he noted that enforcement has become increasingly difficult.
He recommended systemic improvements to ease the stress caregivers face.
“Electronic medical records can reduce the running around to collect results. Improved drug supply and efficient payment systems will also reduce the burden on caregivers,” Akande said.
Sleeping zones, WASH facilities a must – Advocate
Adebusoye recommended immediate, low-cost measures hospitals can adopt while working toward building standard caregiver lodges. These include functional hand-washing points at wards, clean gender-segregated toilets with running water, brief infection-control orientations for visitors, improved mosquito control and ventilation, and converting unused halls into supervised night spaces with bunks, lockers, drinking water and lights-out schedules.
He also outlined medium-term steps such as constructing dedicated “Patient Attendants’ Quarters” with male and female rooms, bathing and laundry points, security and affordable fees with waivers for indigent families. He urged hospitals to align such facilities with Nigeria’s WASH-in-Health Care Facilities guidelines and to adopt tools like WASH-FIT for routine quality checks.
He proposed policies for hospital authorities, including mandatory caregiver lodging, minimum WASH standards, designated sleeping zones (with a ban on corridor sleeping), regular fumigation, ventilated waiting areas and clear feedback channels for reporting poor hygiene or unsafe conditions.
“We cannot claim to be practising patient-centred care while caregivers are sleeping under staircases. The evidence is clear: poor sanitation and sleep deprivation weaken immunity and fuel infections. Providing safe caregiver spaces is essential to protecting both patients and the people looking after them,” Adebusoye said.
Caregivers at risk of anxiety – Psychologist
Speaking on the psychological toll of prolonged caregiving in hospitals, the Head of Clinical Psychology at Intersect Consortium, Alexander Agara, said many relatives face stress that far exceeds infection risk.
He said, “Long-term caregiving in stressful hospital settings commonly causes chronic stress that goes far beyond infection risk, producing anxiety, depression, sleep disturbance, physical health decline, social isolation, financial strain, reduced work performance and, for some, symptoms like PTSD or complicated grief.”
Agara explained that caregiving is a prolonged stressor that increases the likelihood of anxiety and depression over time.
Many caregivers, he noted, report emotional exhaustion, hopelessness and poorer quality of life compared to those who are not in caregiving roles.
The clinical psychologist added that sleep disturbance is one of the most common consequences, as caregivers often stay awake for long hours or sleep in uncomfortable places within the hospital. The resulting insomnia and fatigue weaken the immune system and impair concentration. Chronic stress, constant vigilance, and repeated exposure to medical crises, he said, can also lead to burnout and trauma-like reactions.
Beyond the hospital walls, Agara noted that caregiving affects families socially and financially, with many losing social connections, reducing work hours or stopping work entirely while facing out-of-pocket costs that escalate their stress.
He further stressed the importance of early support and shared practical steps families can take. “Families can protect themselves with concrete steps like regular respite, clear role-sharing, training, boundaries and mental-health care,” he said.
Agara also highlighted what hospitals can do to lessen caregiver strain. “Hospitals can help a lot by identifying and supporting caregivers early through assessment, education, liaison staff, respite pathways and referral,” he added.
The clinical psychologist recommended routine caregiver assessments at admission, assigning a caregiver liaison, structured training with written or visual materials, coordinated respite options and quick referral pathways for mental health support. Flexible visiting and family inclusion in care discussions, he noted, can also reduce confusion and ease post-discharge stress.
Efforts to get the response of the management of UCH to the claims were abortive as the Public Relations Officer asked our correspondent to send the questions to her WhatsApp line with a promise to get the response of the Provost. But it has yet to be received as of press time.
PUNCH NEWS.